Healing Your Child's Eczema Naturally
The American Academy of Dermatology estimates that 10-20% of children suffer from eczema and 20% of infants will experience it at some point. All parents know that baby rashes are common, but what if your child’s rash is getting worse and causing them pain or discomfort.
Unfortunately, conventional medicine says that there is no cure for eczema. I’m sharing the story of my son, Jasper, in hopes that it may help other parents find relief from a root cause, functional perspective.
When Jasper was a few months old we noticed a small dry patch of skin on his chest. It seemed to come and go with no real pattern, but never worsened. Soon he developed another patch of the dry skin on his stomach and I decided it was time to get a second opinion. We asked his pediatrician, a functional family practice physician, as well as a naturopathic doctor about what they thought might be happening.
The family practice doctor said it was a simple case of eczema - nothing to worry about and provided no further recommendations at that time. The naturopathic doctor said it didn’t appear to be eczema, but perhaps was a fatty acid deficiency as the skin is composed of fatty acids. They recommended we give him a probiotic to support gut health, infant fish oil for DHA, and use beef tallow on his skin to provide relief for the dryness.
Within a few months, the rash began to spread all over Jasper’s torso, arms, and legs. Since he is breastfed, I changed my diet to remove gluten, dairy, nuts, soy, eggs, and anything I thought might be contributing to his flare ups. The pattern would look like a big flare where the rash became red, raised and inflamed for a few days, followed by it calming down and becoming very dry and rough. It got worse in the evenings and with heat (such as wearing warm clothes or bathing) causing increased the redness. Each time a flare up would occur, the rash would spread to a new area. He was getting increasingly uncomfortable and itchy.
Before his rash really got out of control, we had visited Hawaii and ate a lot of raw fish (a known source for parasite exposure) and wondered if he may have contracted an infection during that trip.
Below is what his rash looked like as it progressed.
Photo taken December 11, 2021
Photo taken December 29, 2021
Photo taken February 1, 2022
Photo taken February 4, 2022
As things got worse, we returned to his pediatric family practice doctor to seek guidance. She recommended doing a food allergen test and celiac panel. An IgE comprehensive food panel and celiac panel were ordered, which is a blood draw. I want to mention here that drawing blood on an 11 month old is challenging and not a great first option if it can be avoided. While we were hesitant to do the draw, we were desperate for answers.
All testing came back negative. He had no true food allergens or celiac disease. It was a relief, but also left us in the dark once again. It also left his doctor in the dark and she had no further answers for us, referring us to a pediatric dermatologist. When we mentioned running a GI MAP to screen for pathogens, she told us “he was too young to have any pathogens.”
Left without answers, and with the knowledge that he did not have a true food allergy, I took over care for him.
Here’s exactly what we did.
Understanding the Rashes (And Eczema) Are an Internal Imbalance
Any time we think of children’s rashes, we need to be looking internally.
There is a large industry centered around topical solutions for eczema that don’t focus on the root cause of the issue but instead provide symptomatic relief for children (sometimes). Common conventional treatments include topical steroids for eczema, but these also don’t address the root cause and have been linked to several long-term effects for children and suppress the skin’s response that indicates a need for digestive support. Eczema and rashes serve as a red flag that something in our children isn’t functioning properly, and by solely utilizing topical treatments, our children continue to have digestive issues but without symptoms which can lead to long-term health consequences.
One of the primary roles of the skin is to serve as a detoxifications pathway for the digestive system. In other words, when an imbalance is present in the digestive tract, the skin will attempt to detox from pathogens and food intolerances, which typically presents in the form of a rash.
One of the more functional routes in conventional medicine is to look at true food allergies (aka IgE food allergies) but it’s not uncommon for all tests to come back negative. Histamine reactions in the body look similar to food allergens, causing swelling or redness around the eyes, a runny nose, hives or skin rashes, itching, and trouble sleeping. Histamine intolerance falls into the category of food intolerance and children may react to even small amounts of trigger foods without having a true allergy to them.
Just because an IgE food allergen panel comes back negative does not mean that the immune system is not being engaged. Rashes are a sign of mast cell activation, which we’ll discuss more below.
First Steps to Finding Relief
First things first, we ordered a GI MAP stool test. It’s a single sample collection stool test that screens not only for beneficial bacteria in the gut but also dysbiotic (or harmful) bacteria related to general dysbiosis as well as autoimmune triggers, yeast, fungus, and parasites. The GI MAP also measures intestinal health markers that indicate levels of fat and carbohydrate chemical digestion, the gut’s immune response levels and immune response to gluten, liver health, and inflammation. You can see a full list of everything the GI MAP looks at here.
Getting results back for the GI MAP takes 10-14 business days, so in the meantime, we began doing a few other things to provide relief by looking at our diet and what we could reduce to provide symptomatic relief.
Mast cells are a type of white blood cell important for mounting an immune response to an allergen. They are scattered throughout the connective tissue of the body, especially beneath the surface of the skin, near blood vessels and lymphatic vessels, within nerves, throughout the respiratory system, and in the digestive and urinary tracts. They store a number of chemical mediators, one of which is histamine. When we see rashes and eczema in children, their mast cells have been activated by a trigger and are releasing a mediator to mount an immune response. In many cases, this mediator is histamine in relation to eczema.
Histamine intolerance doesn’t always look like a food bothering a child from day one. Instead, think of histamine intolerance as a cup. Every time the body releases histamine, a drop is added to that cup until eventually the cup begins to overflow and a response is generated.
It became clear that his mast cells had become activated in response to something in the body, whether that was pathogenic or a food, so we decided to lower the amount of histamine his body was producing by decreasing the foods known to increase histamine levels. Since he is breastfed, we both adopted a low-histamine diet.
High histamine foods include:
Avocado
Alcohol
Fermented foods and beverages (kefir, yogurt, sauerkraut, kombucha, etc)
Dried fruits
Eggplant
Spinach
Shellfish
Aged cheese
Dairy
We also removed foods that can trigger the release of histamine, which include:
Wheat germ
Bananas
Tomato
Beans
Papaya
Chocolate
Citrus fruits
Nuts
Food dyes and additives
We also removed the probiotic he was taking, which was Klaire Labs Infant Probiotic because some of the strains present in that probiotic can contribute to histamine production and potential overload, to include:
Lactobacillus casei
Lactobacillus delbrueckii subsp. bulgaricus
Lactobacillus helveticus
Streptococcus thermophilus
We had also coincidentally begun increasing his probiotic consumption following our Hawaii trip which coincided with the drastic increases in his rash. These strains are found in some popular infant probiotics, such as :
Klaire Labs Infant Powder
BioGaia Protectis
Gerber Soothe Colic Drops
We immediately switched him to a probiotic that encourages the breakdown of histamine, Smidge Infant Probiotic, and I changed my own probiotic from Microbiome Lab’s MegaSporeBiotic to Seeking Health’s Probiota HistaminX.
Next, we wanted to encourage the breakdown of histamine in the body naturally while reducing triggers. Diamine oxidase (DAO) is a digestive enzyme responsible for the breakdown of histamine in the body. DAO deficiency can lead to an inability to breakdown foods high in histamine, creating an immune response in the gut and body. DAO deficiency is also linked to skin issues such as eczema, hives and psoriasis.
We both started taking desiccated beef liver from Perfect Supplements to support DAO production. We also increased his consumption of salmon and olive oil, both of which support DAO production.
To support the immune system to find homeostasis, we also started giving him Pure Synergy Pure Radiance C sourced from whole food to provide vitamin C without the symptoms the tic abs orbit acid in addition to the fruits and veggies in his diet.
The GI MAP Results
About two weeks later, we received his GI MAP results. At that point in time, we had already started seeing improvement in his skin. There were fewer flare-ups and they were more mild in intensity, lasting shorter durations.
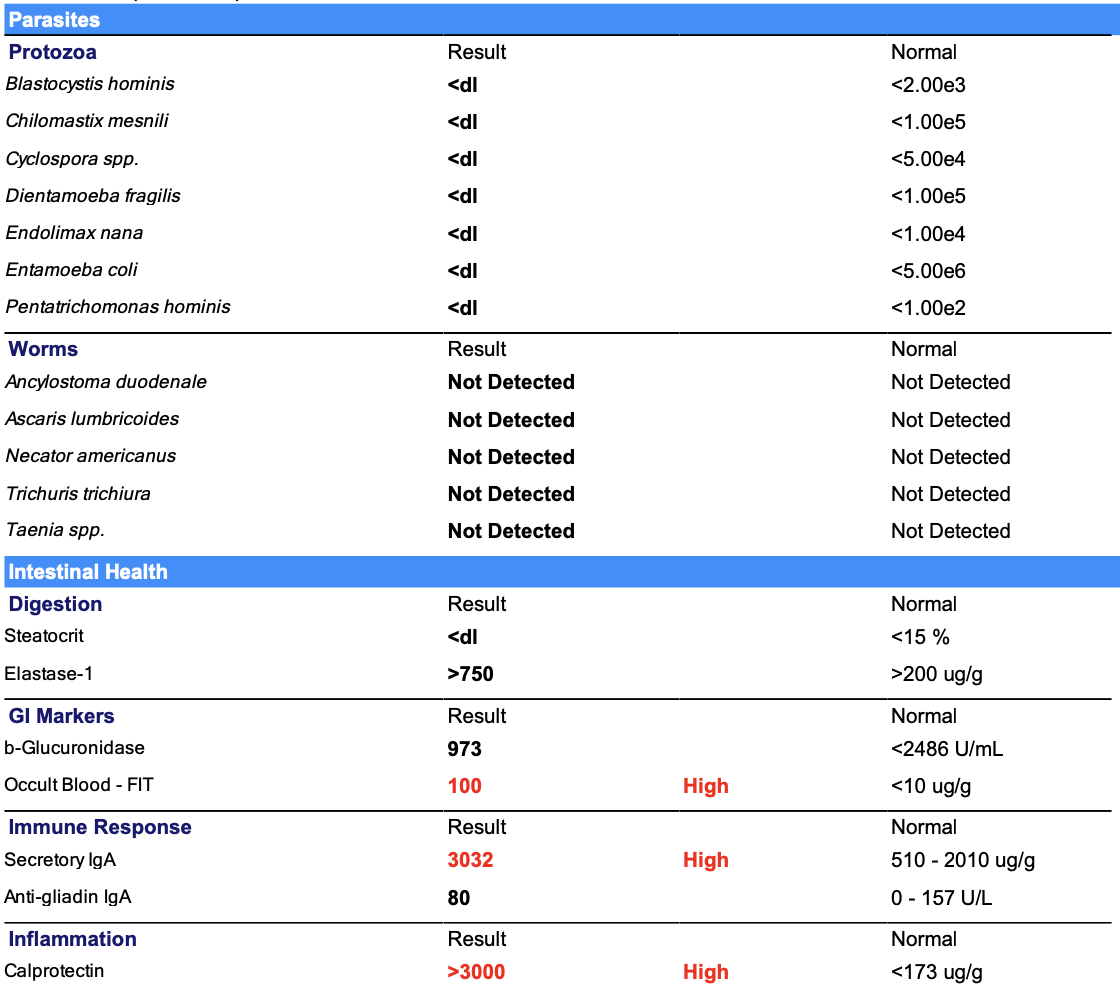
His results were fairly alarming and not what I expected to find.
Here’s what was indicated by his GI MAP:
High C. difficile Toxins A & B
Present helicobacter pylori
High beneficial bacteria (to include Lactobacillus, Escherichia, Clostridia, Bacteroidetes and Firmicutes
High dysbiotic bacteria (to include Bacillus, Enterococcus faecalis, Enterococcus faecium, Staphylococcus aureus, Streptococcus, Methanobacteriaceae
High potential autoimmune trigger bacteria (to include Klebsiella)
High occult blood
High Secretory IgA
High Calprotectin
While all of this may look overwhelming, the overarching interpretation is that he has a bacterial overgrowth in the digestive tract. The fact that it was found both in the stomach (indicated by the h. pylori) as well as the large intestine (indicated by the dysbiotic bacteria) leaves room to believe that it also populated the small intestine. While the GI MAP does not test directly for SIBO (small intestinal bacterial overgrowth), there was reason to believe this could be the case.
Parasites did not show up on his GI MAP. However, I rarely see parasites show up on GI MAP stool tests even when they are present for clients experience classic parasitic infection symptoms. When we see the possibility of SIBO, especially in young children, we have to ask why this bacteria is overgrowing at such drastic rates at such a young age. For us, parasites made sense for creating this dysbiosis due to our diet and trip to Hawaii lining up with the flare of symptoms and the rash being exacerbated.
The high occult blood, secretory IgA and calprotectin indicated that something in his (or my diet) was bothering him. The stool sample was collected prior to starting the low-histamine diet, so while we were making progress there was reason to believe that we were missing a key food trigger.
We decided to run MRT food sensitivity test on both of us. This is a blood panel that tests for any mediator reactions to 170 different food and food chemicals. You can see a sample MRT here. When we went to be drawn, we were able to draw mine but the phlebotomist was unable to draw blood from Jasper, so we decided to start with my results first as he is still breastfed in addition to eating solid foods. At some point in time we may reconsider having his blood drawn to have conclusive results.
We found that a number of foods I was eating regularly (such as chicken, egg yolks, and tomato) were moderately to high reactive for me and were putting stress on my gut immune system which in turn could be putting stress on his GI tract as well even though these were not causing me symptoms.
I also ran a GI MAP on myself to ensure that there was not dysbiosis present in my gut that was contributing to his overall bacteria load since we know that 100,000 bacteria per milliliter of breastmilk are transferred to nursing babies. My GI MAP came back clean and showed that I was not contributing to his dysbiosis. This also helped rule out the possibility that I had a bacterial overgrowth or SIBO that may have been passed onto him in utero, during birth, or via breastfeeding.
What Our Protocol Looked Like
Please note: This is the protocol I put together for Jasper based on his unique circumstances, symptoms and results from his GI MAP in combination with years of digestive healing experience. I am not including dosage here because dosage is extremely important to ensure safety, especially when it comes to children. This information should not be perceived as medical advice and I am happy to discuss creating a personalized protocol for you or your child in a one-on-one setting. You can learn more about working together here.
CellCore Para 1 - Made from 100% pure Mimosa pudica seed, this product functions similar to chia seeds in that it becomes gelatinous when it comes into contact with water. As it makes its way through the GI tract, it scrubs the gut of intestinal buildups, supports the gut microbiome, and promotes the body’s natural ability to detoxify.
CellCore Para 2 - This product is formulated with a variety of herbs (Amla, clove bud, holarrhena, neem, triphala, and vidanga) to support immunity and the gut microbiome, support bowel regularity and balance the but bacteria. This is also an anti parasitic agent.
Sovereign Silver Colloidal Silver - This colloidal silver contains 10 ppm silver hydrosol in purified water. Colloidal silver is commonly utilized for immune support but it is also a strong antimicrobial agent. It’s available in both liquid drops as well as a spray.
Biocidin - Biocidin is a synergistic combination of botanicals that support healthy digestion and elimination and has antimicrobial properties. For GI support, it is best utilized in liquid drops.
CellCore BioToxin Binder - This utilizes CellCore’s carbon technology to provide systemic detoxification, while also supporting cellular repair and increased energy production. It’s a gentle binder that does not need to be taken away from food or other supplements and does not deplete the body of minerals.
Perfect Supplements Desiccated Beef Liver - This beef liver supplement is derived from grass-fed cattle in New Zealand and if filled with bioavailable B vitamins to support liver function and detoxification, as well as providing a source of vitamin A, Beef liver consumption also promoters the production of DAO for histamine breakdown.
Pure Synergy Pure Radiance C - Vitamin C derived from camu camu, acerola and amla, sourced from berries and contains zero synthetic ascorbic acid. This whole foods Vitamin C supports a healthy immune response.
CellCore CT-Minerals - Sourced from the soil and decomposed plant life, this product contains 69 naturally occurring minerals and fulvic acid to support cellular hydration and optimize nutrient absorption.
Nordic Naturals Infant DHA - Contains 100% Artic cod oil to support healthy DHA levels for reducing inflammation systemically.
Smidge Infant Probiotic - Contains seven clinically-proven probiotic strains that are naturally found in healthy infants to help colonize the intestinal tract. It also supports healthy digestion, immunity, and can help with a variety of common baby digestive issues like reflux (GERD), occasional diarrhea and constipation, and even skin issues like eczema without producing histamine.
We’ll plan on doing some of these products for 4 weeks while others will remain in place for 12 weeks to ensure eradication of the dysbiotic bacteria in the gut. Some of these products may stay in rotation long-term to support overall health as well. After we finish an eradication protocol, we’ll also do a GI MAP re-test to ensure balance has been restored to the microbiome.
The Results
Two days after we started eradication, Jasper passed multiple helminths (parasites) varying in length between 1-5 inches. His bowel movements also became more regular.
Two weeks after we began eradication, Jasper’s skin was nearly back to normal and you would never know that he had once been covered in red or dry patches of skin.
His skin flares had completely stopped occurring. He no longer experienced red, inflamed patches of skin across his torso and limbs. Those patches became dry and we used Primally Pure’s Baby Balm to nourish and hydrate the skin as the patches healed, and his skin is now smooth.
His skin looked as though nothing had occurred as new cells began generating.
Photo taken February 24, 2022
Photo taken March 4, 2022
Why Avoiding Food May Not Be The Answer Long-Term
First, elimination diets such as a low-histamine diet can be difficult to follow. While following this type of diet may provide some immediate symptomatic relief, it may be difficult, if not impossible, to follow long term for you and/or your child. Completely avoiding foods that contain histamine may also set them up to develop an inability to process histamine when they inevitably release histamine when coming into contain with these foods later in life.
For this reason, supporting the body with DAO production in combination with reducing the triggers can be the best option. When we support the digestive tract by promoting the proliferation of beneficial bacteria as well as the production of enzymes to breakdown histamine, we can support long-term health in children.
Any time we address pathogens and/or food intolerances in the gut, the goal is to reintroduce foods. The MRT test indicates foods that are causing the release of mediators. By calming the immune system, addressing pathogens, and providing a break from foods causing these reactions, we have an opportunity to heal the gut so that it can potentially withstand these foods again in the future.
It’s also important to avoid instilling any food fear for children. Removing these foods is a temporary solution to provide relief while addressing the root cause and promoting healing. At some point, slow reintroduction of foods can be beneficial to ensure children are able to eat a wide variety of foods filled with vitamins and minerals.
Where To Start
If you’re concerned about your child’s eczema and rashes, I understand the distress you’re feeling right now. If you’re reading this desperate to find relief for your little one, trust your gut and keep digging. We found pathogens lurking in his digestive system even though we were told it wasn’t possible. We found relief without buying every topical cream on the market or needing topical steroids. Holistic, root cause care for eczema is possible when we look internally at the GI tract, liver, and immune system to support them accordingly.
Here’s a step by step guide to find relief and address the root cause:
Reduce their histamine load and any foods known to bother them
Some common foods to reduce/eliminate include dairy, gluten and soy.
Remove histamine producing probiotics if either of you are using a probiotic.
Experiment with a low histamine diet.
Consider their breastfeeding status
If they are exclusively breastfed, looking at your own digestion and food intolerances is the best place to start.
If they are breastfed but old enough that they are consuming solid foods as well, it can be beneficial to look at the diet for both of you to determine your bio-individual food intolerances and digestive concerns.
If they are not breastfed, use formula, or are simply at the age where they are eating exclusively solid foods, looking at their diet is key to determine anything that be irritating their gut.
Consider a GI MAP for your child at a bare minimum
Collecting a stool sample from a young child is relatively easy and will provide a lot of information about their digestive health. I recommend this for any child experiencing rashes or eczema to determine what may need rebalancing in the microbiome.
This can be a good starting point. The Secretary IgA marker on the GI MAP may indicate a need to know more about food sensitivities, warranting a MRT test for either them or you (if breastfed).
Consider a MRT food sensitivities test
This is a blood draw so it’s not always a great option for young children, but will provide invaluable information on the foods that are reactive for them to take the guesswork out of dietary restrictions
For children who’s immune system is engaged to fight off pathogens or in the event of intestinal permeability, food sensitivities information can ensure they see less skin irritations by reducing the overlap stress load on the GI system and body as a whole. If you’re seeing an immune response mounted per the GI MAP without the presence of pathogens, it may be time to look at all immune cells being mounted in response to food rather than only the IgE panel which looks only at true food allergens.
Work with someone who understands not only how to interpret the testing you choose to utilize but can create a comprehensive protocol that is both safe and effective for your little one. These tests are only as valuable as the interpretation of them.
If you’re looking for guidance, please reach out for a complimentary consultation to discuss what’s happening and how I may be able to help by email me at deidre@always-growing.com. We work with clients virtually all over the US and internationally, but can only order the GI MAP for clients working with us as a client.









Deidre founded Always Growing Nutrition in 2015 with an enthusiasm for health, fitness, and understanding how to optimize the human body. She approaches nutrition from the perspective that each body is unique and this is key to creating nutrition programs that are sustainable for each person to maintain long-term, but also programs that work.
Her passions lie in digestive and hormone health, and she loves working with clients who struggle with balancing these complex systems. She believes that everyone deserves personalized nutrition, to understand how their body works, and to have the support to get answers about their health. She has worked with hundreds of clients to create a body they love with food they love.
When she's not working with clients, you'll find her enjoying everything Colorado has to offer from hiking to camping to craft beers.